GOITER REMOVAL SURGERY COST IN INDIA
GOITER REMOVAL SURGERY COST IN INDIA
- Introduction
- Symptoms
- Risk Factor
- Preparation
- Procedure
- Post Procedure
- Success Rate
- FAQS
- Top Doctors
- Top Hospitals
GOITER REMOVAL SURGERY COST IN INDIA
Duration of Treatment
usually takes 2 to 3 hours
Days of Stay
usually two days in the hospital and 5 days outside the hospital.
Anesthesia
General anesthesia
Cost
3000 to 5000 USD
How much does Goiter Removal Surgery Cost in India?
“Looking Goiter Removal Surgery Cost in India at best thyroid surgery hospitals at an affordable cost in different cities like Delhi, Mumbai, Chennai, Kolkata, and Bangalore? Here, we answer the question and explain how to choose the top thyroid surgeons in India for better results; our surgeon did more than 1000 transplants successfully.
- Goiter Removal Surgery Cost: starting from #3,000 to $5,000 USD.
- Hotel Cost Near Hospital – starting from $18 to $50 USD (as per hotel services).
- Food Cost – starting from $20 to $30 USD (per day).
- Miscellaneous cost – $20 USD (per day).
- It’s an only rough estimate, final treatment will plan after the fresh evaluation reports.
- In India, Goiter Removal Surgery Cost can vary as per the diagnosis, patient’s conditions, ENT surgeon experience, Implant quality, hospital facilities, and city.
- To make an appointment, learn more about thyroid surgery, read below information, or call / WhatsApp/ Viber – our experts to answer at +91 9513357762. Still, have questions? call our expert team SUBMIT ENQUIRY
Who is the best Thyroid surgeons in India?
- Dr. Ameet Kishore
- Dr. W.V.B.S. Ramalingam
- Dr. Sanjay Sachdeva
- Dr. Vijay Verma
- Dr. Atul Kumar Mittal
- Dr. A Muraleedharan
- Dr. Prateek Nayak
- Dr. Harpreet Singh
- Dr. Sanjucta Ghosh Arora
- Dr. B. P Sharma
Which is the best hospital for Thyroid Surgery in India?
- ARTEMIS HOSPITAL
- MANIPAL HOSPITAL
- FORTIS HOSPITAL
- MEDANTA HOSPITAL
- YASHODHA HOSPITAL
- GLOBAL HOSPITAL
- APOLLO HOSPITAL
- NARAYANA HOSPITAL
Why you choose Us for Thyroid surgery in India?
We are one of the best health care services providers for more than 10 years of experience to provide the best treatment at an affordable cost and guide our international patients to choose the top destination as per patient’s budget and treatment.
- Comprehensive and 100% transparency.
- Help to Choose the Best Option for ENT Treatment.
- Based on the highest international standard.
- Qualified ENT surgeon – For more success rate of surgery.
- Affordable Cost – Save your money on procedures
- Professionalism – The best care and transparency on treatment.
- Patient Safety – Using high-quality of services for zero infection.
What is Goiter (Thyroid) Surgery?
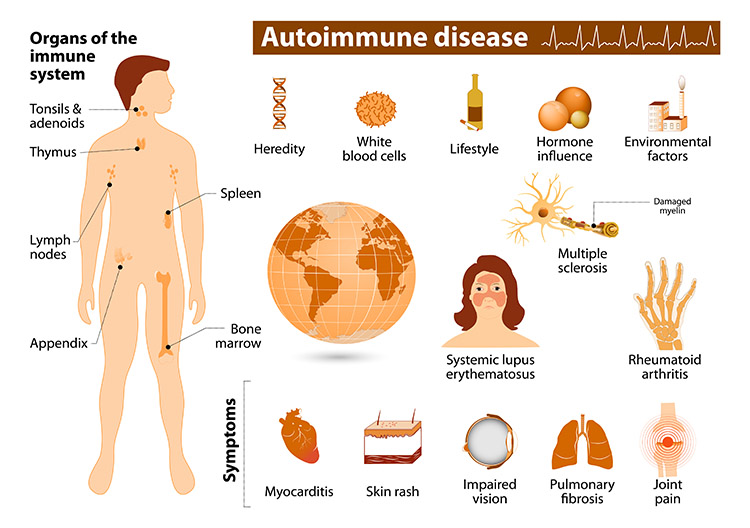
Goiter refers to abnormal enlargement of the thyroid gland. The thyroid is a butterfly-shaped gland located in the lower part of the neck. The most common cause of goiters is a lack of iodine in the diet. Goiter can occur when the thyroid gland is inefficient thyroid hormones, inflamed, occupied by tumors.
Types of goiter-
- Diffuse goiter
- Nodular goiter
- Nontoxic goiter
- Toxic goiter
Still, have questions? call our expert team
What are the Signs and Symptoms of Goiter removal?
- Large goiters
- cause breathing difficulties or swallowing
- Multinodular goiters
- swelling on neck
- Coughing
What are the Risk factors of Goiter removal surgery?
- Risks of anesthesia
- Bleeding
- Infection
- Temporary dizziness
- Nerve Damage
- Parathyroid gland damage
How to prepare for Goiter removal surgery?
- For ENT patient is required to go for PSC ( Pre-surgery check-up ) to do some blood test, ECG and ECH for Cardiac check-up and urine tests to know he /she is fit for surgery or not.
- Before the operation, you’ll be asked to sign a consent form, which gives the surgeon permission to carry out the treatment.
- The doctor should be informed about any medication that the patient may be taking.
- The patient is admitted to the hospital on the same days before the procedures and advised to remain empty stomach/Fasting.
- Thinners medicines have to stop before ten days of surgery.
- The best Goiter (Thyroid) Surgery cost in India starting from 3000 to 5000 USD the cost varies depending upon City, hospitals, surgeon’s qualifications & experience.
What are the best procedures for Goiter Removal Surgery?
Goiter treatment depends upon the size of the goiter, signs, and symptoms. The ENT doctor will advise as per patient condition –
- Medications.
- Surgery.
- Radioactive iodine
Before surgery, the surgeon and anesthesia doctors will guide you about the benefits and risk factors of Goiter removal surgery.
Step 1 – Anesthesia: Goiter removal surgery takes 2 to 3 hours depending upon the procedures by giving general anesthesia to relieve pain.
Step 2 – The incision: The ENT surgeon makes an incision of 3 to 4 inches long at the base of your neck by using magnifying lenses. The surgeon removes all or part of the thyroid gland (total or partial thyroidectomy) is depending on the patient condition. Surgery is also the treatment for thyroid cancer.
Step 3 – Closing the incisions: The ENT surgeon flaps the skin after the surgery with the help of Sutures, skin adhesives, tapes or clips that close the skin incisions.
What is the post-op care for Goiter removal surgery?
The doctor will give complete information about post care of surgery, regarding recovery; proper caring of incisions, taking medications and managing. Stitches or staples will be removed after 7 to 10 days of surgery. If only part of the thyroid removed that might not need thyroid hormone replacement medicine. And some medication you have to take life.
What is the success rate of Goiter removal?
Goiter removal surgery is usually safe and the success rate is more than 98% depending on the patient, surgeon experience.
FAQS FROM DOCTOR
What Question Ask before Goiter Removal Surgery?
- Are you a board-certified ENT surgeon in India?
- Does your hospital certify to perform ENT surgery?
- Am I a good patient for you to Goiter removal surgery?
- Let me know success rates and how long time will take for recovery?
- What are the risk factors for surgery?
- What treatment plan do you recommend and Why?
- What are the advantages and disadvantages of surgery?
- What are the costs involved with Goiter removal surgery?
- How will a long time take for surgery?
- How should I prepare for Goiter removal surgery?
- How long I have to say in the hospital and outside the hospital?
- How long will it take to recover from Goiter removal surgery?
- When can I go for normal activities, including exercise?
- Do I have stitches, staples, and/or bandages after surgery?
- Do I have a scar or other permanent effects from the surgery?
- Do I need any follow-up appointments or tests after?
- Facebook
- Twitter
- Linkedin
- Whatsapp
- Telegram
- Viber
- Line